PRP Injections
What is Platelet Rich Plasma?
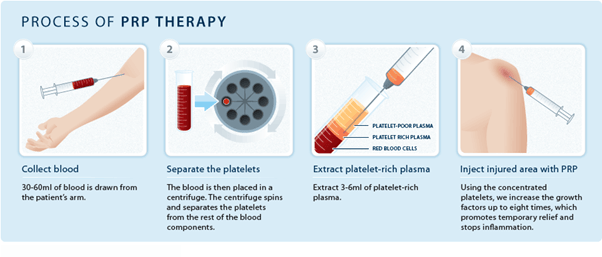
Platelet rich plasma is a blood product, drawn from your body, which has a high concentration of platelets that release various growth factors.[1–3]
These growth factors are thought to have a beneficial effect in tissue healing, and more recently the white blood cells have been thought to provide both anti-inflammatory and ant-infective effects.[4-6] Sports Physicians use PRP as an adjunctive tool to rehab.[7]
What is the Evidence for PRP Treatment?
Currently there are only a few studies of adequate quality that show that PRP is effective for early knee osteoarthritis[8-10], however there is more evidence than for arthroscopic surgery of the knee.[11–13] Studies comparing it to other injections for arthritis of the knee have showed it is superior.[13–16] At this stage there are no predictors of who will respond to each of these injections, and the sensible approach seems to be to use them judiciously to facilitate realistic functional goals. Compared to Cortisone injections, PRP injections don’t seem to delay recovery or increase recurrence of tendon disorders including plantar fasciitis, tennis elbow, rotator cuff problems and jumpers knee.[17–27]
Why are Platelet Rich Plasma Injections Used?
PRP is used to augment the healing process, particularly in areas of the body where there is slow tissue repair and turnover. High white cell counts appear advantageous in soft tissue and tendon disorders,[6,28-30] while multiple injections with low white cell counts are better for joint pain.[4,9]
Will PRP Work for My Problem?
PRP has potential benefits for the right problem in the right patient. It is only one part of the whole management regime for any problem. Despite all the research, overall the current evidence-base for PRP is at high risk of bias.[11,31,32] However, it is very safe and a temporary post-injection flare of symptoms is the most likely adverse effect.[4,33]
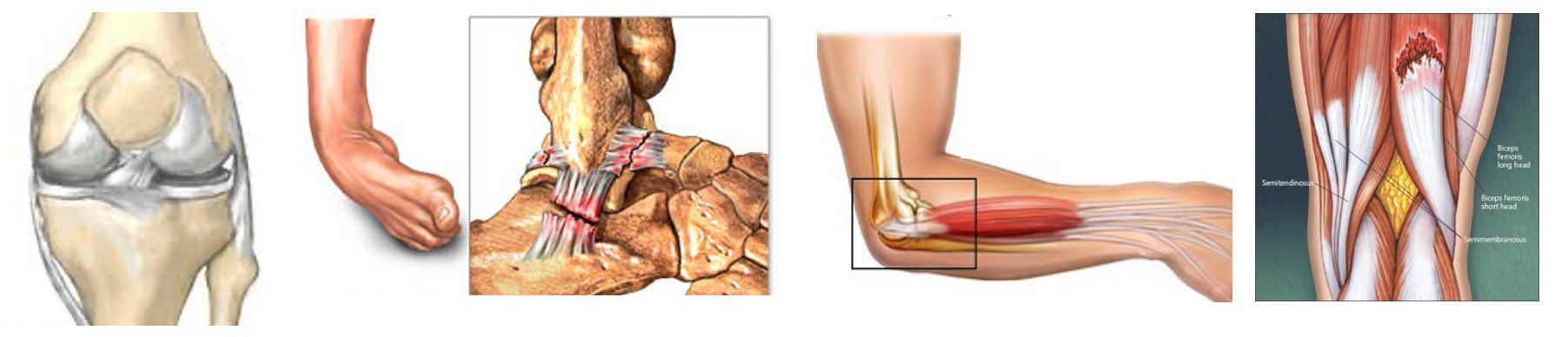
Other specific problems that PRP appears to be effective for include:
- Ankle syndesmosis injuries (and similar ligament injuries with poor healing)
- Horizontal meniscal tears of the knee
- Slow healing muscle injuries involving the tendon (hamstring, quadriceps)
- Chronic tendon pain- such as patella, achilles, elbow and gluteal tendons
- Chronic plantar fasciitis
- Early osteoarthritis of the hip
How Much Does PRP Cost?
The out of pocket cost is usually significantly less than this when done by a Sports Physician. It ranges from $300-$900 each, and overall costs depend on the type of PRP used and the number of injections recommended. Sports physicians provide a holistic service within the context of understanding the overall problem. When combined with optimisation of diet and exercise, patients are much more likely to experience benefit.
What are the Risks?
The main risks are considered the same as any other injection. There is an estimated 1 in 20,000 chance of infection or significant bleeding. These risks are minimised through the use of a sterile technique and an ultrasound to guide the safest course for the needle. About 5% of patients experience a flare of the pain can last 24-48 hours but this is very manageable with analgesia and rest.
What Should I Expect?
The whole process takes between 20-30 minutes. First, about 10-15mL of your blood is drawn from your arm. Then that blood is centrifuged for 10 minutes. The PRP is then extracted, and injected under ultrasound guidance after the area is cleaned. Local anaesthetic is sometimes used but never in the same injection as the PRP as this destroys the platelets. Anti-inflammatory medications (Celebrex, Mobic, Voltaren etc) should be stopped 3 days prior to injection, and for 2 days afterwards, because these impair platelet function.
You should plan to rest the injected area for 2-3 days following the injection. Depending on the site of the injection, this may involve getting driven to your appointment, wearing a protective sling, boot or other device.
Platelet Rich Plasma Injections Treatment Process
Preparation for Treatment
- Take your medical history,
- Conduct a physical examination, and
- You may be asked to have a number of tests to ensure that the injections are suitable.
- Advise the doctor if you are taking Aspirin or Blood-thinning medications, regardless of whether you are expecting to have treatment or just a consultation.
- Stop any anti-inflammatory medications.
Day of Your Treatment
- Do not consume large amounts of alcohol for at least 24 hours prior to treatment
- Do not use Anti-inflammatory medications for 72 hours prior to treatment (eg Ibuprofen)
- Avoid vigorous physical activity or exercise for 24 hours,
- Wear loose clothing
Injection Approach
The injection is generally performed with an initial local numbing medication (local anesthetic) via a very small needle. This allows the PRP then to be injected very accurately under ultrasound-guidance, without pain.
During Your Treatment
This procedure can be carried out in minutes at the doctor’s office. The patient is:
- either made to sit or lie down, while the doctor then administers the Platelet Rich Plasma Injection.
- may feel a burning or pinching sensation that goes away quickly.
In some cases, your doctor may use ultrasound guidance for more accurate needle placement when required.
After Your Treatment
Patients are given clear post-injection written instructions. Most patients:
- Are able to walk, drive and return home afterwards without issue
- Should rest the injected area for a day before resuming normal activities.
- Avoid any strenuous activities such as heavy lifting or exercises for a week.
If local pain at the injection site your doctor
- may prescribe pain relief medication.
- Recommend using a cold compresses to alleviate symptoms.
Common Questions
Reference List
1. Perez, A. G. M. et al. Relevant Aspects of Centrifugation Step in the Preparation of Platelet-Rich-Plasma. Int. Sch. Res. Not. 2014, e176060 (2014).
2. Amable, P. R. et al. Platelet-rich-plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Res. Ther. 4, 67 (2013).
3. Kushida, S. et al. Platelet and growth factor concentrations in activated platelet-rich-plasma: a comparison of seven commercial separation systems. J. Artif. Organs Off. J. Jpn. Soc. Artif. Organs 17, 186–192 (2014).
4. Riboh, J. C., Saltzman, B. M., Yanke, A. B., Fortier, L. & Cole, B. J. Effect of Leukocyte Concentration on the Efficacy of Platelet-Rich-Plasma in the Treatment of Knee Osteoarthritis. Am. J. Sports Med. 44, 792–800 (2016).
5. Fitzpatrick, J., Bulsara, M. K., McCrory, P. R., Richardson, M. D. & Zheng, M. H. Analysis of Platelet-Rich-Plasma Extraction. Orthop. J. Sports Med. 5, (2017).
6. Fitzpatrick, J., Bulsara, M. & Zheng, M. H. The Effectiveness of Platelet-Rich-Plasma in the Treatment of Tendinopathy A Meta-analysis of Randomized Controlled Clinical Trials. Am. J. Sports Med. 0363546516643716 (2016) doi:10.1177/0363546516643716.
7. Samra, D. J. & Orchard, J. W. Patterns of platelet-rich-plasma use among Australasian sports physicians. BMJ Open Sport Exerc. Med. 1, e000054 (2015).
8. Patel, S., Dhillon, M. S., Aggarwal, S., Marwaha, N. & Jain, A. Treatment with platelet-rich-plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am. J. Sports Med. 41, 356–364 (2013).
9. Görmeli, G. et al. Multiple P-R-P injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 25, 958–965 (2017).
10. Tietze, D. C., Geissler, K. & Borchers, J. The effects of platelet-rich-plasma in the treatment of large-joint osteoarthritis: a systematic review. Phys. Sportsmed. 42, 27–37 (2014).
11. Meheux, C. J., McCulloch, P. C., Lintner, D. M., Varner, K. E. & Harris, J. D. Efficacy of Intra-articular Platelet-Rich-Plasma Injections in Knee Osteoarthritis: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. (2015) doi:10.1016/j.arthro.2015.08.005.
12. Sihvonen, R. et al. Arthroscopic Partial Meniscectomy versus Sham Surgery for a Degenerative Meniscal Tear. N. Engl. J. Med. 369, 2515–2524 (2013).
13. Buchbinder, R. & Harris, I. A. Arthroscopy to treat osteoarthritis of the knee? Med. J. Aust. 199, 100 (2013).
14. Ayhan, E., Kesmezacar, H. & Akgun, I. Intraarticular injections (corticosteroid, hyaluronic acid, platelet-rich-plasma) for the knee osteoarthritis. World J. Orthop. 5, 351–361 (2014).
15. Campbell, K. A. et al. Is Local Viscosupplementation Injection Clinically Superior to Other Therapies in the Treatment of Osteoarthritis of the Knee: A Systematic Review of Overlapping Meta-analyses. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. (2015) doi:10.1016/j.arthro.2015.03.030.
16. Campbell, K. A. et al. Does Intra-articular Platelet-Rich-Plasma Injection Provide Clinically Superior Outcomes Compared With Other Therapies in the Treatment of Knee Osteoarthritis? A Systematic Review of Overlapping Meta-analyses. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. (2015) doi:10.1016/j.arthro.2015.03.041.
17. Hart, L. Corticosteroid and Other Injections in the Management of Tendinopathies: A Review. Clin. J. Sport Med. 21, 540–541 (2011).
18. Bisset, L. et al. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. BMJ 333, 939 (2006).
19. Nichols, A. W. Complications associated with the use of corticosteroids in the treatment of athletic injuries. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 15, 370–375 (2005).
20. David, J. A., Sankarapandian, V., Christopher, P. R., Chatterjee, A. & Macaden, A. S. Injected corticosteroids for treating plantar heel pain in adults. Cochrane Database Syst. Rev. 6, CD009348 (2017).
21. Jain, K., Murphy, P. N. & Clough, T. M. Platelet -rich-plasma versus corticosteroid injection for plantar fasciitis: A comparative study. Foot Edinb. Scotl. 25, 235–237 (2015).
22. Mishra, A. K. et al. Efficacy of Platelet-Rich-Plasma for Chronic Tennis Elbow A Double-Blind, Prospective, Multicenter, Randomized Controlled Trial of 230 Patients. Am. J. Sports Med. 42, 463–471 (2014).
23. Filardo, G. et al. Platelet-rich-plasma intra-articular injections for cartilage degeneration and osteoarthritis: single- versus double-spinning approach. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 20, 2082–2091 (2012).
24. Behera, P., Dhillon, M., Aggarwal, S., Marwaha, N. & Prakash, M. Leukocyte-poor platelet-rich-plasma versus bupivacaine for recalcitrant lateral epicondylar tendinopathy. J. Orthop. Surg. Hong Kong 23, 6–10 (2015).
25. Almeida, A. M. de et al. Patellar Tendon Healing With Platelet-Rich-Plasma A Prospective Randomized Controlled Trial. Am. J. Sports Med. 40, 1282–1288 (2012).
26. Dragoo, J. L., Wasterlain, A. S., Braun, H. J. & Nead, K. T. Platelet-rich-plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am. J. Sports Med. 42, 610–618 (2014).
27. Wang, A. et al. Do Postoperative Platelet-Rich-Plasma Injections Accelerate Early Tendon Healing and Functional Recovery After Arthroscopic Supraspinatus Repair? A Randomized Controlled Trial. Am. J. Sports Med. 43, 1430–1437 (2015).
28. Samra, D. J. et al. Effectiveness of a single platelet-rich-plasma injection to promote recovery in rugby players with ankle syndesmosis injury. BMJ Open Sport Exerc. Med. 1, e000033 (2015).
29. Laver, L. et al. Plasma-rich in growth factors (PRGF) as a treatment for high ankle sprain in elite athletes: a randomized control trial. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 23, 3383–3392 (2015).
30. Podesta, L., Crow, S. A., Volkmer, D., Bert, T. & Yocum, L. A. Treatment of Partial Ulnar Collateral Ligament Tears in the Elbow With Platelet-Rich-Plasma. Am. J. Sports Med. 41, 1689–1694 (2013).
31. Miller, L. E., Parrish, W. R., Roides, B. & Bhattacharyya, S. Efficacy of platelet-rich-plasma injections for symptomatic tendinopathy: systematic review and meta-analysis of randomised injection-controlled trials. BMJ Open Sport Exerc. Med. 3, e000237 (2017).
32. Laudy, A. B. M., Bakker, E. W. P., Rekers, M. & Moen, M. H. Efficacy of platelet-rich-plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br. J. Sports Med. 49, 657–672 (2015).
33. Nguyen, C. & Rannou, F. The safety of intra-articular injections for the treatment of knee osteoarthritis: a critical narrative review. Expert Opin. Drug Saf. 16, 897–902 (2017).
34. Zhang, W. et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr. Cartil. OARS Osteoarthr. Res. Soc. 16, 137–162 (2008).