Ultrasound-Guided Cortisone Injections
What are Cortisone Injections?
Cortisone is a synthetic form of a Cortisol, a natural hormone your body produces. Cortisol is also called the “coping hormone” because it increases during times of stress and assists with regulating the immune system and energy systems to cope with the demands of life.
Cortisone (injectable corticosteroid) is a potent anti-inflammatory and tends to be useful to treat problems related to excessive inflammation. However, it the important thing to understand about cortisone is that it is a “catabolic steroid”. This is the opposite of “anabolic steroid”, meaning it tends to shrink everything down. It powerfully reduces inflammation- and this is good- but is also inhibits the signals around an injured area that assist healing. Cortisone Injections are used to reduce pain, swelling and stiffness. They do not heal injured tissue.
The first study to demonstrate potential harmful effects was published by an Australian physio in 2000. Bisset (2006) showed that patients who were treated with a cortisone injection for tennis elbow had worse results that the patients who had no treatment (a wait and see approach).[1]
Because of this cortisone has a bad reputation for the treatment of chronic injuries.[2-4] We now avoid using it in most tendon disorders.
However, just like any tool, cortisone is very helpful when used in the right situation. It still has a role for acute injuries where the inflammation is excessive, or in chronic injuries where pain, stiffness or swelling impedes rehabilitation.
What are the Advantages of Cortisone Injections?
Cortisone injections work on several levels and are most noted for reducing inflammation and relieving pain. The advantages of Cortisone Injections are that that they are:
- Minimally-invasive,
- Non-surgical,
- Fast-acting, and
- Very effective.
When Should I Consider a Cortisone Injection?
Cortisone Injections are only required if first line medication and physical therapy have been unable to relieve pain and swelling.
The main purpose of this treatment is to improve the quality of life for the patient and provide relief.
Where there is a lot of inflammation and swelling, cortisone is helpful.
- Simple ankle sprains with lots of swelling and pain
- The fat pad of the knee
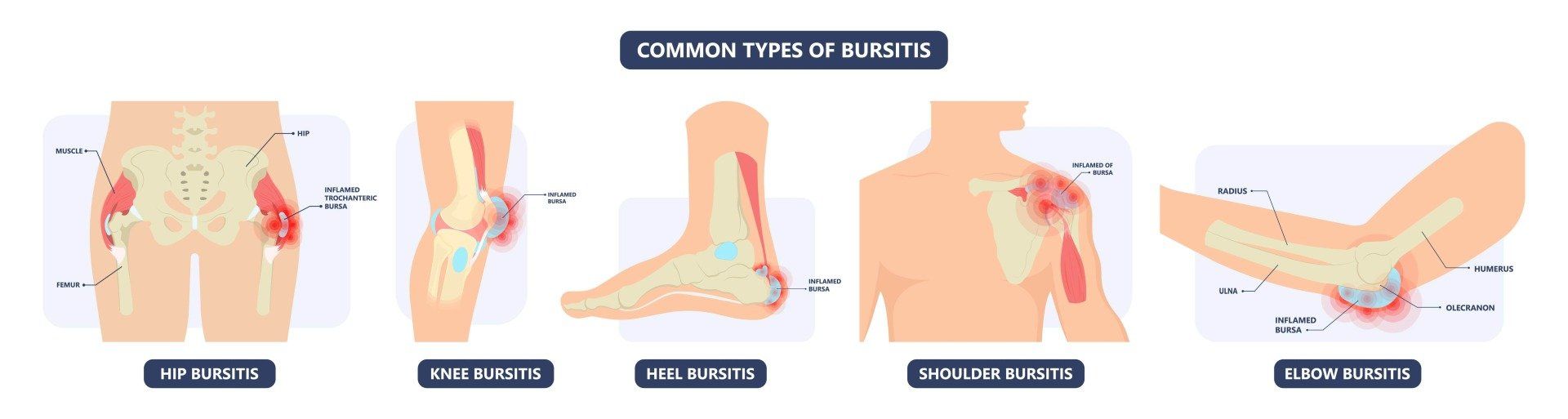
- Inflamed bursa (sacs of lubricating fluid)- knee, elbow or elsewhere.
- Frozen or pinching (impinged) shoulder [6]
- Carpal tunnel syndrome [7]
- Nerve roots in the back (for “sciatica”) [8]
- Joint OA and tendon pain, when balancing the benefits and harms
- You should avoid having a cortisone injection into a chronic tendon injury like tennis elbow or achilles tendinosis [3,5] There are better, less harmful options to treat these.
The effects of the injection usually last from several weeks to three months and provide a window of opportunity for physical therapists to assist with healing of the damaged joint or tendon.
How is Cortisone Administered?
The skin is prepared using an antiseptic agent to reduce risk of infection.
The degree of discomfort during the procedure is generally mild as the needle used is fine (thin) and local anaesthetic is usually mixed in with cortisone.
The needle is then guided into the relevant body part using an ultrasound (unless the area being injected is very close to the skin and ultrasound wouldn’t help to prove the exact location of the injection). The guidance allows the cortisone to be accurately delivered into the area of suspected/proven pain.
What are the Risks? What Happens After the Injection?
The risks of cortisone injection are the same as for any injection into a joint- namely- infection and bleeding. These are both in the order of 1 in 80,000 injections. After a cortisone injection and once the local anaesthetic wears off (2-4 hours) there may be a temporary flare in pain for the first 24-48 hours, and this usually responds well to ice and rest. If pain at the site persists beyond this time, please return for medical review.
Generalised symptoms may also occur including facial flushing, mood disturbance, sleep disturbance and menstrual disturbance. These are uncommon, short-lived and resolve spontaneously, but if you have had the response previously, then there is a higher chance of recurrence. Localised skin depigmentation (lightening of colour) may occur with shallow injections, especially in patients with darker skin. Tendon rupture can occur with cortisone injections directly into a tendon, and this should be avoided.
You should plan to rest the injected are for 5-7 days (strictly for 24 hours) following the injection. Depending on the site of injection, this rest may involve getting driven to and from your appointment, wearing a protective sling, boot or other device.
Cortisone Injection Treatment Process
Preparation for Treatment
In order to prepare for the treatment, the patient should be adequately counselled to ensure that the informed consent is obtained and the treatment is understood.
The Doctor will:
- Take your medical history,
- Conduct a physical examination, and
- You may be asked to have a number of tests to ensure that the injections are suitable.
- Advise the doctor if you are taking Aspirin, Anti-inflammatory or Blood-thinning medications, regardless of whether you are expecting to have treatment or just a consultation.
Day of Your Treatment
- Do not consume large amounts of alcohol for at least 24 hours prior to treatment,
- Avoid vigorous physical activity or exercise for 24 hours,
- Wear loose clothing
Injection Approach
In some cases, the doctor may recommend a
local numbing medication be applied to the injection site, this also temporarily relieves pain. This can be discussed.
During Your Treatment
This procedure can be carried out in minutes at the doctor’s office. The patient is:
- either made to sit or lie down, while the doctor then administers the Cortisone Injection.
- may feel a burning or pinching sensation that goes away quickly.
The best results have been shown to occur when the injection is performed under ultrasound guidance.
- Higher concentrations can be administered safely with minimal side-effects, allowing anti-inflammatory properties to work to their full potential.
After Your Treatment
You will be given written post-injection Instructions.
Check with the Practice Manager regarding whether you-
- Are able to walk or drive afterwards without issue.
- Can work the same day.
- Need to rest the injected area.
Where there is local pain, the patient is advised to rest for 2 days before resuming normal activities, and up to 4-5 days before resuming any formal exercise.
Common Questions
Reference List
1. Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. BMJ. 2006 Nov 4;333(7575):939.
2. Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet Lond Engl. 2010 Nov 20;376(9754):1751–67.
3. Dean BJF, Lostis E, Oakley T, Rombach I, Morrey ME, Carr AJ. The risks and benefits of glucocorticoid treatment for tendinopathy: a systematic review of the effects of local glucocorticoid on tendon. Semin Arthritis Rheum. 2014 Feb;43(4):570–6.
4. Nichols AW. Complications associated with the use of corticosteroids in the treatment of athletic injuries. Clin J Sport Med Off J Can Acad Sport Med. 2005 Sep;15(5):370–5.
5. Hart L. Corticosteroid and other injections in the management of tendinopathies: a review. Clin J Sport Med Off J Can Acad Sport Med. 2011 Nov;21(6):540–1.
6. Wu T, Song HX, Dong Y, Li JH. Ultrasound-guided versus blind subacromial-subdeltoid bursa injection in adults with shoulder pain: A systematic review and meta-analysis. Semin Arthritis Rheum. 2015 Dec;45(3):374–8.
7. Habib GS, Badarny S, Rawashdeh H. A novel approach of local corticosteroid injection for the treatment of carpal tunnel syndrome. Clin Rheumatol. 2006 May;25(3):338–40.
8. Manchikanti L, Cash KA, Pampati V, Falco FJE. Transforaminal epidural injections in chronic lumbar disc herniation: a randomized, double-blind, active-control trial. Pain Physician. 2014 Aug;17(4):E489–501.