Bursitis
What Is Bursitis?
Swelling and inflammation near a joint may be a sign of bursitis, a condition that involves a buildup of liquid and inflammation in a bursa sac that cushions a joint.
Bursitis is also commonly known as housemaid’s knee, student’s elbow, and tailor’s bottom, to name a few.
Where Are Bursa Sacs?
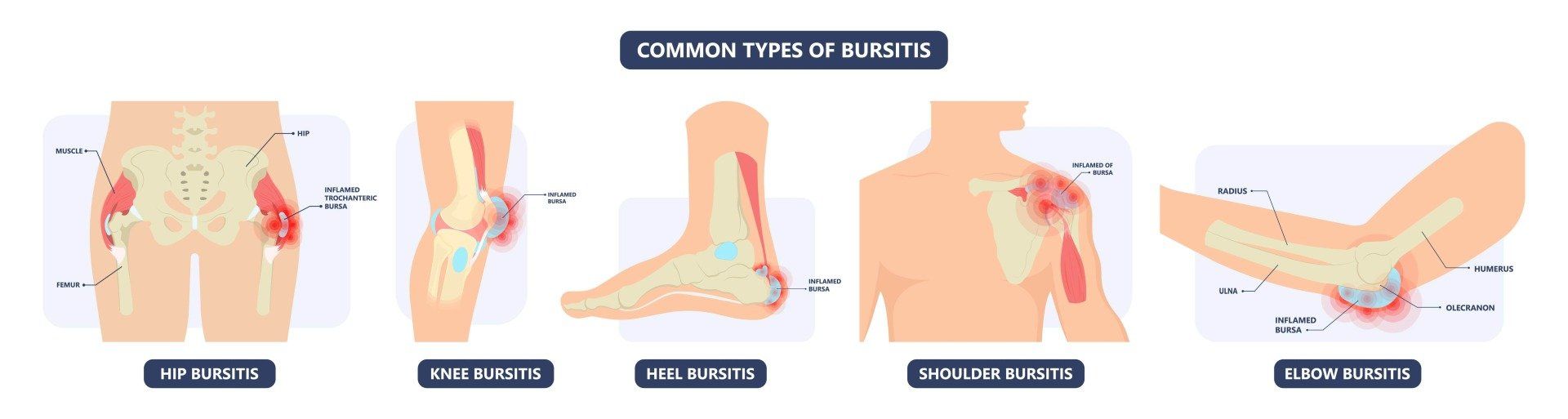
A bursa is a “potential space” which develops between two layers of tissue that move across each other that would otherwise create friction. Usually, they are microscopically thin but they can fill with fluid either as a normal process to protect from friction or due problems such as inflammation or infection.
Everyone has bursas throughout their body. The knee has at least 6 and sometimes up to 13 bursas around it.
Some bursas exist in everyone – like the one that protects the rotator cuff in the shoulder. Others can develop as a protective response to friction (like in the front of the foot) or as a response to infection or injury.
There are approximately 160 bursae in the body, only a handful of them usually cause bursitis.
Bursa Sacs are thin, slippery sac found around a joint that serves to reduce friction between bone and surrounding soft tissue, such as skin, muscles, ligaments and tendons. A bursa sac is made up of a synovial membrane, or synovium, that produces and contains synovial fluid.
The most common bursa sacs that cause Bursitis are found in the knee, shoulder, elbow, and hip. Less frequently, bursitis may also occur in the heel, wrist, buttocks, back and big toe.
Why Does an Enlarged Bursa Mean?
Firstly, there is no absolute consensus in ‘normal’ bursa sizes. An enlarged bursa can be a completely painless and normal process to protect from friction.
An example is that swimmers have large bursas in their shoulders to protect them from repetitive shoulder movements. Seeing an enlarged bursa on a scan does not mean the cause of the pain has been found!! An enlarged bursa can mean,
- A normal process responding to normal friction
- A normal response to abnormal friction (an injury, bone spur or weakness leading to the extra friction)
- Response to direct trauma (typically at the knee and elbow bursas)
- A pathological process such as infection or even gout
What Causes Bursitis?
Bursitis may result from one or more of the following events:
- Trauma or Injury to the point of a bone - including falling, bumping, or lying for an extended period
- Overuse due to play or work activities causing injury to the joint area - including running up stairs, climbing, or standing for long periods of time,
- Incorrect posture - resulting from scoliosis, arthritis of the lumbar spine, and other spinal problems
- Soft Tissue Stress - abnormal or poorly positioned joint or bone (leg length discrepancies or arthritis in a joint)
- Previous Surgery - may cause scar tissue that can contribute to bursitis
- Bone Spurs - or calcium deposits in the tendons that attach to the bone.
Other conditions like rheumatoid arthritis, gout, and psoriasis that can irritate the synovium and cause it to become inflamed. The inflamed synovium will thicken and produce excess synovial fluid and can cause symptoms such as localized swelling, skin redness and warmth, tenderness and pain.
Bursitis is more common in women and in middle-aged or elderly people.
Why Does Bursitis Cause Pain?
Many types of bursitis cause no pain at all (even when there is a lot of swelling). Bursitis can cause pain when it leads to excessive inflammation, infection or compression that stops surrounding structures from working normally. Sometimes bursitis appears painful because it is a part of a more widespread problem like greater trochanteric pain syndrome or shoulder impingement.
Symptoms of Bursitis
Typically, bursitis causes local pain around the affected joint:
- at the point of bone, radiating outside and around the area
- when walking upstairs, squatting or related activities
- during activities where the affected joint is being engaged
- when lying on the affected side
- when pressure is on the affected area
In the early stages, the pain is usually described as sharp and intense.
Later on, the pain may become more of an ache and spread across a larger area of the joint region.
Diagnosis of Bursitis
Patients who suspect they have a bursa sac injury or inflammation should seek a medical consultation. The diagnosis of Bursitis can often include:
Physical Examination
A doctor may evaluate the affected joint to determine the presence of swelling, a limited range of motion, abrasions, bruising, or other common signs of a Bursitis.
Throughout the process, your doctor is likely to inquire as to how the injury was sustained, the level of pain the athlete is in, and what symptoms have been identified.
Obtain a Full Medical History
Your doctor will ask about your symptoms, medical history, any sports participation and activities that aggravate your condition.
Prior injury can elevate an athlete’s risk of sustaining Bursitis. With this in mind, your doctor will likely evaluate the patient’s medical history in order to determine if a former condition has increased the likelihood of a given injury being present.
Medical Imaging
Once your doctor has completed the physical examination of the affected area, medical imaging such as an X-ray or Magnetic Resonance Imaging (MRI) can help to form a final diagnosis.
A comprehensive evaluation of the patient’s joint allows Dr Samra to eliminate various possibilities, arrive at a diagnosis, and recommend a treatment plan.
Treatment for Bursitis
Treatment for Bursitis can begin immediately after the injury is sustained. Common first-response treatments for Bursitis may include:
- Pain medication - nonsteroidal anti-inflammatory medications (NSAIDs) can relieve some pain or discomfort associated with Bursitis (ibuprofen or naproxen)
- POLICE - To reduce the pain and swelling surrounding the injured area.
- Protect - support and position the injury in a way that doesn't worsen it.
- Optimal Loading - rehabilitation begins as soon as the injury occurs. It is a matter of finding non-exacerbating load to stimulate and enhance tissue recovery.
- Ice - for comfort and pain relief. 10 minutes as often as every 4-6 hours for the first 2 days.
- Compression - to control swelling and inflammation.
- Elevation - the most potent means of reducing swelling is lifting the limb above the level of the heart.
Pausing athletic activity until the symptoms of Bursitis have faded.
Recommended Treatments for Bursitis
Following a medical evaluation, your doctor will be able to recommend a course of treatment. Common treatments for Bursitis include:
- Exercise training: A physician or physical therapist may recommend exercise training and bracing to strengthen the associated tendon and reduce the symptoms of Bursitis. This process commonly involves having an athlete engage in a series of helpful exercises.
- Bracing: A physician may recommend stabilizing the patella with either a brace or athletic tape to keep it in place during exercise training.
- Taping: An adhesive tape is applied over affected joint, to alter the joints alignment and movement.
- Orthotics: Special shoe inserts may be prescribed for those with flat feet that may help relieve the pain.
- Injection Therapies: In more advanced cases of patellar tendinopathy, it is common for physicians to recommend injection therapies. In these treatments, an athlete is given an injection (typically corticosteroids) to reduce inflammation and accelerate the healing of the patellar tendon.
- Platelet-rich plasma therapy: This practice, also known as PRP, involves injecting the site of the injury with the patient's own platelet-rich plasma in an effort to accelerate healing.
- Dry needling: In dry needling, a needle without a syringe is inserted into the affected area and moved, with the guidance of an arthroscopic camera, in an effort to break up or destroy degenerative structures within the joint that may be contributing to injury.
- Hyperthermia thermotherapy: This process involves using both a heating source and a cooling source to raise the temperature of internally damaged tissues (in this case the patellar tendon) while allowing the surface level tissues to stay cool.
- Extracorporeal shockwave treatment: This procedure, also known as ESWT, involves sending sound energy impulses into the source of tissue irritation. The force from the sound waves penetrate solid tissues well and can diminish pain-producing inflammatory chemicals and stimulate the immune response to clear damaged or torn soft tissues.
A patient may need to undergo other treatments but a holistic approach with a focus on strengthening is always required.
How is Bursitis Treated?
The treatment for bursitis depends entirely on the type and the cause. Many cases of bursitis are a normal response to trauma or friction and need no treatment at all. Sometimes an inflammatory bursitis needs to be treated first so that the underlying cause can be addressed – this is often true in the shoulder or hip where a
corticosteroid injection (cortisone) can reduce the pain and inflammation long enough to correct the underlying problems. Infective bursitis is entirely different and should never be treated with a corticosteroid injection which can worsen the problem. A correct diagnosis, antibiotic treatment and sometimes even a surgical washout can be required in these cases.