Frozen Shoulder
What is Frozen Shoulder?
Adhesive capsulitis is a very unique and very painful condition that involves immunological changes inside the shoulder joint that lead to deposition of irregular collagen tissue in the shoulder capsule associated with pain and stiffness that rapidly worsens over a few months, then stabilizes over a few months, then gradually resolves over several months.
The shoulder is a complex ball-and-socket joint that allows full movement of the arm.
It offers a wide range of motion, but also makes it vulnerable to injury.
The capsule of the shoulder has layers of collagen tissue that stabilize the shoulder joint at ends of range, and an inner lining that produces joint lubricating fluid called synovial fluid.
This capsule normally has some extra slack down the bottom- this area called the inferior glenohumeral ligament, but instead of being thin like a plastic bag, this tissue becomes thick and leathery, which creates stiffness and quite severe pain in the early stages when that tissue is stretched. It is thought that this process are triggered by an immune response with infiltration of cells that lay down excessive collagen called fibroblasts being responsible for the stiffness , while chronic inflammatory cells and new blood vessels and nerves growing into the thickened capsule are thought to be responsible for the marked pain.1
Frozen Shoulder (adhesive capsulitis) causes pain, stiffness and a loss of motion in your shoulder. Shoulder pains begin slowly until there is a marked loss of motion in the shoulder.
Typically the course of the frozen shoulder occurs in three different phases that last about 6-9 months each. Rarely it can last up to 3 years. Frozen Shoulder (adhesive capsulitis), is pain, stiffness and a loss of motion in your shoulder. Shoulder pains begin slowly until there is a complete loss of motion in the shoulder.
- Freezing stage (red)
- The patient develops a slow onset of pain. As the pain worsens, the shoulder loses motion.
- Frozen stage (blue) - The patient experiences a slow improvement in pain, but the stiffness remains.
- Thawing stage (green)- the patient slowly regains full mobilisation of their shoulder as it returns to normal.
Causes of Frozen Shoulder
We aren’t entirely sure why Frozen Shoulder occurs; however, it is more likely to occur in patients who recently had to immobilize their shoulder for a long period or trauma (after surgery or an arm fracture).
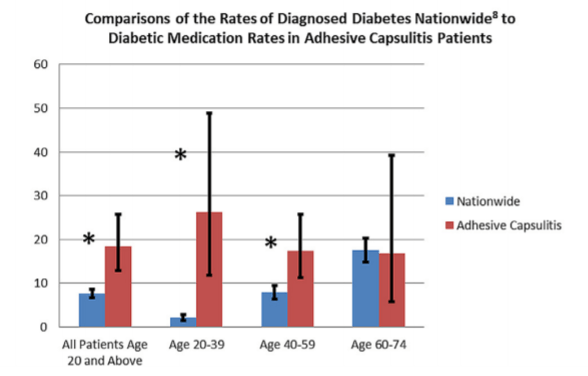
There is an association with auto-immune conditions such as Hashimoto’s and Graves Thyroiditis, Type 1 diabetes, Celiac disease and Pernicious anemia (the so-called thyro-gastric cluster). 2 The strongest association is with Type 2 Diabetes (and Insulin Resistance or "Pre-Diabetes") 3–5
Frozen shoulder is also associated with Heart Disease and cardiac surgery, Parkinson’s Disease, Breast Cancer (post-surgery).
Frozen Shoulder Symptoms
Frozen Shoulder tends to cause a background of Dull, Aching Pain With sharper shoots of Pain occurring with sudden movements and shoots down the front and side of the arm.
Lack of mobility- especially loss of rotation and elevation (patients often notice inability to reach behind their back first).
Diagnosis of Frozen Shoulder
Often, Frozen Shoulder can be identified during a physical exam, but further testing may pick up on important contributors and overlapping conditions such as diabetes, osteoarthritis, rotator cuff tears and impingement syndromes.
This process starts with Consultation including a comprehensive history, examination and possibly a point of care ultrasound
- Further testing can include
- X-rays – Dense structures, such as bone, show up clearly on x-rays. X-rays may show other problems in the shoulder, such as osteoarthritis.
- MRI – provides high resolution, panoramic, detailed images of the soft tissues. An MRI can produce cross-sectional images of internal structures required if the diagnosis is unclear. 7
- Ultrasound is a dynamic test that can allow us to examine the shoulder during movement at the time of consultation. One key finding in a frozen shoulder is increased blood flow and tissue thickening around the top of the biceps tendon (this is called the “Rotator Interval”). 8
While not all these approaches or tests are required to confirm the diagnosis, this diagnostic process will us to review any possible risks or existing conditions that could affect treatment and recovery.
Treatment for Frozen Shoulder
Nonsurgical treatments
Frozen shoulder generally improves over time without any intervention, however, it can take an average of 2-3 years.9 If symptoms are severe, affecting sleep quality and not controlled by physiotherapy and judiciously prescribed medication, escalation to corticosteroid injections is reasonable. 10,11
- Steroid injections have been shown to be effective for pain in the early phases of a frozen shoulder for reduction of pain. The location of injection is important as bursal cortisone injections do not enter the joint and settle joint related pain
- These injections are delivered to the shoulder joint, often via the rotator interval as well as the bursa and sometimes from the posterior approach as well
- Hydro-dilatation or High-Volume injections have no strong evidence of being superior to cortisone injections but may assist in return of range of motion in the later phases 12–15
- Physical therapy- especially after the painful phase has settled is useful to maintain and restore strength and range of motion 16
Frozen Shoulder Surgery
Surgery for a frozen shoulder is a last resort but has been shown to improve range of motion significantly. 17,18
However, most surgeons do not like to operate in the early stages before the condition has stabilized as surgery is known to cause frozen shoulder. It is thought that the trauma of surgery can stir up further immunological stimulus to make pain and stiffness worse. Therefore, patients tend not to be offered surgery while they are in the freezing phase.
Reference List
1. Fields BKK, Skalski MR, Patel DB, White EA, Tomasian A, Gross JS, et al. Adhesive capsulitis: review of imaging findings, pathophysiology, clinical presentation, and treatment options. Skeletal Radiol. 2019 Aug;48(8):1171–84.
2. Cakir M, Samanci N, Balci N, Balci MK. Musculoskeletal manifestations in patients with thyroid disease: Thyroid disease and musculoskeletal system. Clin Endocrinol (Oxf). 2003 Aug;59(2):162–7.
3. Austin DC, Gans I, Park MJ, Carey JL, Kelly JD. The association of metabolic syndrome markers with adhesive capsulitis. J Shoulder Elbow Surg. 2014 Jul;23(7):1043–51.
4. Pietrzak M. Adhesive capsulitis: An age related symptom of metabolic syndrome and chronic low-grade inflammation? Med Hypotheses. 2016 Mar;88:12–7.
5. Zreik NH, Malik RA, Charalambous CP. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J. 2016 May 19;6(1):26–34.
6. Boyle-Walker KL, Gabard DL, Bietsch E, Masek-VanArsdale DM, Robinson BL. A profile of patients with adhesive capsulitis. J Hand Ther Off J Am Soc Hand Ther. 1997 Sep;10(3):222–8.
7. Zappia M, Di Pietto F, Aliprandi A, Pozza S, De Petro P, Muda A, et al. Multi-modal imaging of adhesive capsulitis of the shoulder. Insights Imaging. 2016 Apr 23;7(3):365–71.
8. Lee JC, Sykes C, Saifuddin A, Connell D. Adhesive capsulitis: sonographic changes in the rotator cuff interval with arthroscopic correlation. Skeletal Radiol. 2005 Sep;34(9):522–7.
9. Manske RC, Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008 May 23;1(3–4):180–9.
10. Ahn K, Jhun H-J, Choi K-M, Lee Y-S. Ultrasound-Guided Interventional Release of Rotator Interval and Posteroinferior Capsule for Adhesive Capsulitis of the Shoulder Using a Specially Designed Needle. Pain Physician. :8.
11. Prestgaard T, Wormgoor MEA, Haugen S, Harstad H, Mowinckel P, Brox JI. Ultrasound-guided intra-articular and rotator interval corticosteroid injections in adhesive capsulitis of the shoulder: a double-blind, sham-controlled randomized study. Pain. 2015 Sep;156(9):1683–91.
12. Catapano M, Mittal N, Adamich J, Kumbhare D, Sangha H. Hydrodilatation With Corticosteroid for the Treatment of Adhesive Capsulitis: A Systematic Review. PM R. 2018 Jun;10(6):623–35.
13. Lee D-H, Yoon S-H, Lee MY, Kwack K-S, Rah UW. Capsule-Preserving Hydrodilatation With Corticosteroid Versus Corticosteroid Injection Alone in Refractory Adhesive Capsulitis of Shoulder: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2017;98(5):815–21.
14. Saltychev M, Laimi K, Virolainen P, Fredericson M. Effectiveness of Hydrodilatation in Adhesive Capsulitis of Shoulder: A Systematic Review And Meta-Analysis. Scand J Surg SJS Off Organ Finn Surg Soc Scand Surg Soc. 2018 May 1;1457496918772367.
15. Yoong P, Duffy S, McKean D, Hujairi NP, Mansour R, Teh JL. Targeted ultrasound-guided hydrodilatation via the rotator interval for adhesive capsulitis. Skeletal Radiol. 2015 May;44(5):703–8.
16. Page MJ, Green S, Kramer S, Johnston RV, McBain B, Chau M, et al. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014 Aug 26;(8):CD011275.
17. Forsythe B, Lavoie-Gagne O, Patel BH, Lu Y, Ritz E, Chahla J, et al. Efficacy of Arthroscopic Surgery in the Management of Adhesive Capsulitis: A Systematic Review and Network Meta-analysis of Randomized Controlled Trials. Arthrosc J Arthrosc Relat Surg. 2021 Jul;37(7):2281–97.
18. Boutefnouchet T, Jordan R, Bhabra G, Modi C, Saithna A. Comparison of outcomes following arthroscopic capsular release for idiopathic, diabetic and secondary shoulder adhesive capsulitis: A Systematic Review. Orthop Traumatol Surg Res OTSR. 2019 Sep;105(5):839–46.