Jumper's Knee
Introduction to Jumper's Knee
Jumper’s Knee is similar to “Runner's Knee”. Jumper’s Knee and Runner’s Knee are common terms often used to describe pain at the front of the knee.
Jumper’s knee refers to a problem in the patellar tendon. These problems and pain can be related to:
- Thickening and wear (patellar tendinosis)
- Accumulation of micro-tears to form a visible tear (more akin to wear)
- Inflammatory chemicals (there are usually NO inflammatory cells in tendons)
As the name suggests, Jumper’s Knee is a common complaint among athletes and people involved in plyometic sports such as netball, basketball, volleyball.
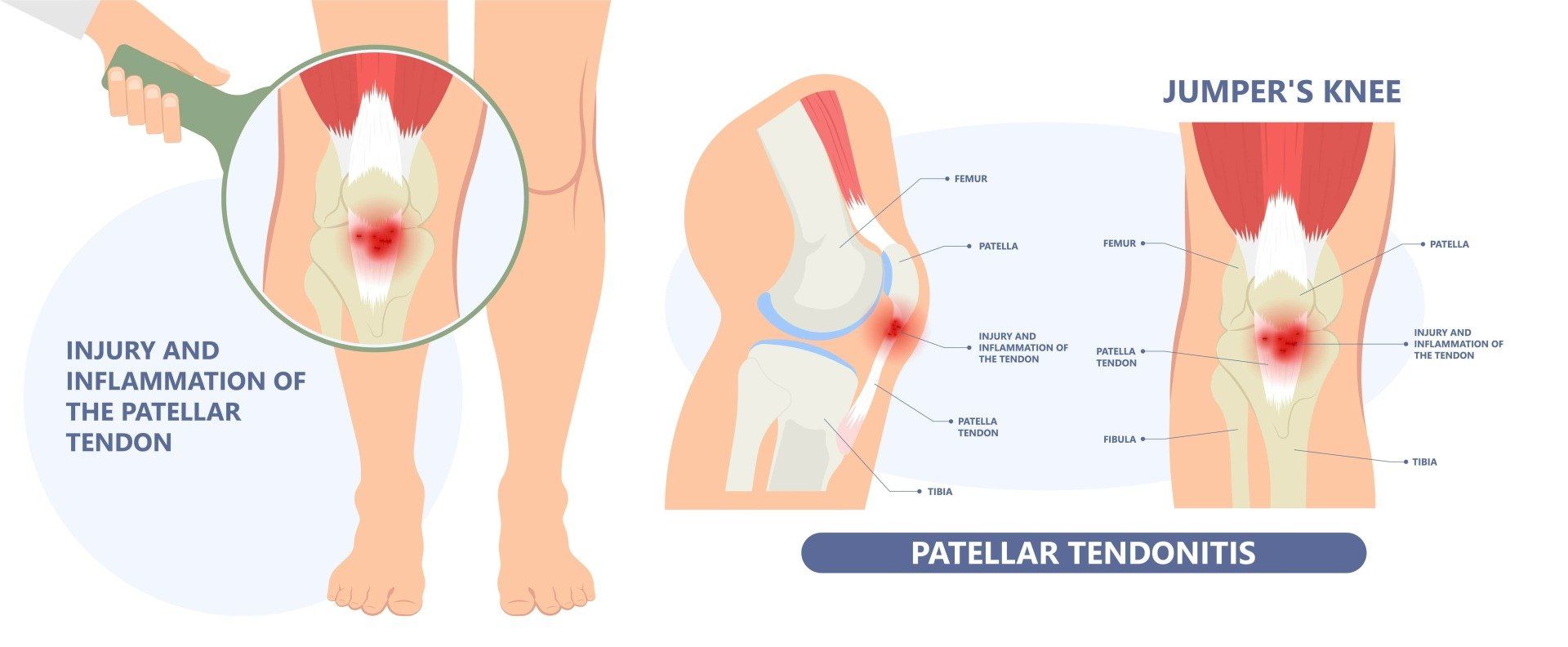
Anatomy of Jumper's Knee
The pain usually occurs under or around the front of the kneecap (patella). You can usually point to the area with one finger.
The patellar tendon begins (or originates) on the patella (kneecap) and travels down the front of the knee to insert on the top of the shin bone, called the tibial tubercle. When the thigh’s quadriceps muscles contract, the patellar tendon is pulled, which in turn straightens the knee and extends the leg.
The kneecap or patella is a sesamoid bone that is embedded in a tendon that connects the muscles of the thigh to the shin bone (tibia). The function of the patella is to protect the front part of the knee.
Causes of Jumper's Knee
The patellar tendon moves every time the knee bends or straightens. Over time, overuse of the knee can cause tiny tears to form within the patellar tendon, which causes the jumper’s Knee. For example, a basketball player who jumps up and down on a parquet floor every day may experience mini-traumas to the patellar tendon that eventually causes painful knee symptoms.
Typically, jumper’s knee is caused by one or all of these factors:
- Overuse or sudden stress on the patellar tendon (such as a heavy or awkward landing) can cause inflammation or tears in the tendon tissue. This may cause pain, swelling, and discomfort, particularly during jumping, running, and other athletic activities.
- Deconditioning from excessive or sudden rest (often due to illness or a separate injury)
- Rigidity of the lower limb due to stiffness of other joints not contributing to shock absorption (e.g hip stiffness)
This can cause the tendon to progress along the "continuum" of tendinopathy, leading to more degenerative changes that are very slow to remodel. With this in mind, athletes who find that the initial symptoms of jumper’s knee are not easing with a few days rest should seek out a medical evaluation to determine the best ways to prevent further injury.
Types of Jumper's Knee
Jumper’s knee can be classified three ways, based on a continuum of pathology
- REACTIVE- acute jumper’s knee - occurring from sudden, unexpected overexertion of the patellar tendon but
- DISREPAIR- continued symptoms that require careful activity modification and load management
- DEGENERATION- chronic jumper’s knee - manifests as a recurring problem over time.
Symptoms of Jumper's Knee
The most common symptom of Jumper’s Knee is a dull aching pain underneath the kneecap while walking up or downstairs, squatting, kneeling down, and sitting with your knees bent for a long period of time.
Individuals with patellar tendinopathy may experience some or all of the following symptoms:
- Pain during athletic motion. An athlete with patellar tendinopathy may feel a sharp, throbbing pain beneath their kneecap during a workout or competition. At first, the pain may worsen with athletic activity and recede with rest. If left untreated, the pain may become constant, present even during times of rest. The pain will be worst when kicking, running, or bending the knee, as these actions activate the patellar tendon.
- The hallmark of patella tendinopathy that distinguishes it from runner's knee is focal, direct tenderness under the knee cap THE SIZE OF ONE OR TWO FINGERS
- Swelling. Like most patellar injuries, jumper’s knee may cause mild swelling of the knee joint. Athletes may notice that their knee looks swollen and has a reduced range of motion.
- Discomfort during daily activities. The patellar tendon helps extend the knee to straighten the leg during daily activities such as kicking, climbing stairs, or bending down. Athletes with advanced cases of patellar tendinopathy may notice increased pain in their knee from daily activities.
Diagnosis of Jumper’s Knee
Patients who suspect they have sustained knee injuries should seek a medical consultation. The diagnosis for a knee injury often include:
A doctor may evaluate the affected part of the knee to determine the presence of swelling, a limited range of motion, abrasions, bruising, or other common signs of a knee injury.
Throughout the process, your doctor is likely to inquire as to how the injury was sustained, the level of pain the athlete is in, and what symptoms have been identified.
Full Medical History and Examination
You will be asked about your symptoms, medical history, any sports participation and activities that aggravate your condition.
Prior injury can elevate an athlete’s risk of sustaining an injury to the knee. With this in mind, the patient’s medical history is fully assessed in order to determine if a former condition has increased the likelihood of a given injury being present.
Your knee will be examined carefully to determine the presence of swelling, a limited range of motion, abrasions, bruising, or other common signs of a knee injury. Your "kinetic chain" will also be assessed to determine if there is any other contributor to overload of the patella tendon.
Medical Imaging
Once an impression is formed, medical imaging such as point-of-care Ultrasound, X-ray or Magnetic Resonance Imaging (MRI) can help to form a final diagnosis.
A comprehensive evaluation of the athlete’s knee allows Dr Samra to eliminate various possibilities, arrive at a diagnosis, and recommend a treatment plan. Neovascularity on ultrasound is a sign that there is new nerve and blood vessel ingrowth into the tendon, which may make you a candidate for
PRP therapy.
The Treatment's for Jumper's Knee
Treatment of jumper’s knee can begin immediately after the injury is sustained. Common first-response treatments for jumper’s knee may include:
- Pain medication - Nonsteroidal anti-inflammatory medications (NSAIDs) can relieve some pain or discomfort associated with jumper’s knee (Ibuprofen or Voltaren)
- POLICE - To reduce the pain and swelling surrounding the injured area.
- Protect - support and position the injury in a way that doesn't worsen it
- Optimal Loading - rehabilitation begins as soon as the injury occurs. It is a matter of finding non-exacerbating load to stimulate and enhance tissue recovery.
- Ice - for comfort and pain relief. 10 minutes as often as every 4-6 hours for the first 2 days.
- Compression - to control swelling and inflammation.
- Elevation - the most potent means of reducing swelling is lifting the limb above the level of the heart.
Modifying athletic activity until the symptoms of jumper’s knee are controlled. It is important to find the right dose or "sweet spot" for exercise to maintain healthy stimulus to the tendon. Prolonged rest is unhelpful because the tendon is not given the mechanical signals to remodel and heal (this is called "mechanotherapy").
Recovery is slow but sure if the correct diagnosis is obtained and the correct stimulus and building blocks for recovery are applied.
Recommended Treatments for Jumper's Knee
A patient may need to undergo other treatments to ensure the ongoing health of the patellar tendon. Following a medical evaluation, your doctor will be able to recommend a course of treatment.
Common treatments for jumper’s knee include:
- Exercise therapy: The single most important treatment is Strengthening exercise to stimulate healing of the patellar tendon and reduce the symptoms of jumper’s knee. This process (called Mechanotherapy) commonly involves having an athlete engage in a series of tendon retraining exercises that are graded from slow, to heavier slow exercise to heavy and fast exercise.
- Movement Coaching: The "Kinetic Chain" refers to the linkages between the joints that produce efficient movement. Inadequate or incoordinated movement of the hips and feet during landing and jumping often reduces load absorption and can therefore lead to overload of the knees. Focusing only on the tendon can mean the big picture is missed, predisposing to recurrent injury.
- Bracing: A physician may recommend stabilizing the patella with either a brace or athletic tape to keep it in place during exercise training.
- Taping: An adhesive tape is applied over the patella, to alter the kneecap alignment and movement. Taping of the patella may reduce pain.
- Orthotics: Special shoe inserts may be prescribed if foot alignment contributes to the pain.
- Dry needling: In dry needling, acupuncture needles are inserted into the affected area and moved, to try to stimulate a healing response.
- Extracorporeal shockwave treatment: This procedure, also known as ESWT, involves sending electric impulses into the muscle tissue surrounding the patella to deliver force to damaged tissues. The force from the electric waves might help induce some tissue healing, but more likely they disrupt pain nerve-endings and desensitise the area to allow effective exercise therapy.
- Injection Therapies: In more advanced cases of patellar tendinopathy, injection therapies are an option. In these treatments, an athlete is given an injection such as P-R-P or prolotherapy. Most doctors now avoid "cortisone" or corticosteroids, which may help initially but are thought to lead to impaired tendon recovery.
- Platelet-rich-plasma-therapy: This practice, also known as P-R-P, involves injecting the site of the injury with a concentrate of a patient's own platelets and white cells in an effort to accelerate healing, and improve pain to promote exercise therapy
A patient may need to undergo other treatments to ensure the ongoing health of the knee, but surgery is an absolute last resort.
Prevention of Jumper's Knee
- If you are overweight, you may need to control your weight to avoid overstressing your knees
- Gradually increase the intensity, duration and frequency of your workouts/jumping sports
- Avoid running on hard surfaces without adequate conditioning
- Wear proper fitting good quality running shoes with good shock absorption
- Avoid running straight down hills; instead, walk down or run in a zigzag pattern
- Optimise the mobility of your spine, hips and ankles to contribute to shock absorption during landing
- Warm-up for 5 minutes before starting any exercise. This should include Isometric hold exercises that may reduce tendon pain quickly
- There is limited evidence for any benefits of stretching, but if it is a routine for you then this does no harm