Achilles Tendinopathy
What Is Achilles Tendinopathy?
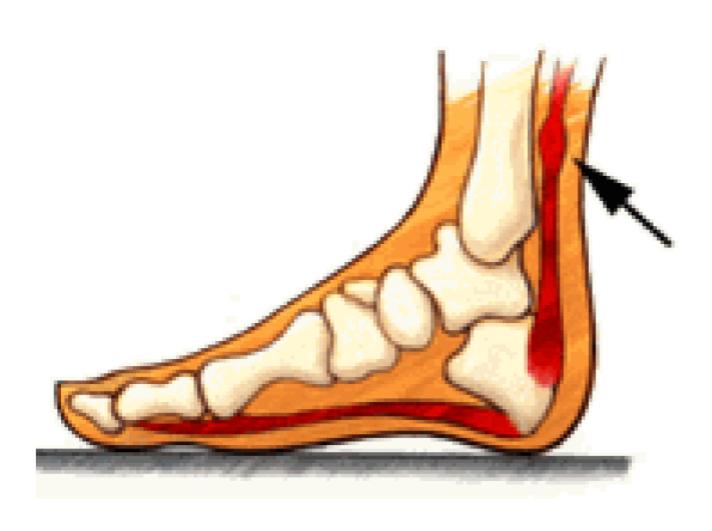
Achilles Tendinopathy is usually an overuse injury that is common especially to joggers and jumpers, due to the repetitive action and so may occur in other activities that require the same repetitive action.
What Causes Tendon Pain?
Tendons are the tough fibres that connect muscle to bone. Most tendon injuries occur near joints, such as the shoulder, elbow, knee, and ankle. A tendon injury may seem to happen suddenly, but usually, it is the result of many tiny tears to the tendon that have happened over time. Health professionals may use different terms to describe a tendon injury.
You may hear:
- Tendonitis (or Tendinitis): This actually means "inflammation of the tendon," but inflammation is rarely the cause of your tendon pain.
- Tendinosis: This refers to tiny tears in the tissue in and around the tendon caused by overuse.
What Causes Achilles Tendinopathy?
Achilles tendinopathy is an overuse injury that is common especially to joggers and jumpers, due to the repetitive action and so may occur in other activities that require the same repetitive action.
Most tendon injuries are the result of gradual wear and tear to the tendon from overuse or ageing. Anyone can have a tendon injury, but people who make the same motions over and over in their jobs, sports, or daily activities are more likely to damage a tendon.
A tendon injury can happen suddenly or little by little. You are more likely to have a sudden injury if the tendon has been weakened over time.
Common Causes of Achilles Tendonitis Include:
- Over-training or unaccustomed use – “too much too soon”
- The excessive intensity or Distance increase
- Change in training surface – e.g. grass to bitumen
- Lack of training variation
- Poorly supportive footwear
- Hill running
Achilles Tendinopathy Risk Factors
- Gender: Men > Women
- Age: >30 most common
- Weight: Higher body weight increases risk
- Diabetes
- Calf Muscle: weakness, poor endurance &/or tightness
- Poor Lower Limb Muscle Control: eg. Poor hip and knee muscle control
- Stiff Ankle/Foot Joints
Symptoms of Achilles Tendinopathy
Achilles tendinopathy may be felt as a burning pain at the beginning of an activity, which gets less during activity and then worsens following activity. The tendon may feel stiffness first thing in the morning or at the beginning of some exercise.
- Achilles tendinopathy usually causes pain, stiffness, and loss of strength in the affected area.
- The pain may get worse when you use your Achilles tendon.
- You may have more pain and stiffness during the night or when you get up in the morning.
- The Achilles may be tender, red, warm, or a swollen lump may be present if there is inflammation.
- Variable pain. Achilles pain can vary significantly depending upon your exercise load.
Achilles tendinopathy is one of many causes of lower calf or heel pain. The correct diagnosis is vital to your treatment plan and recovery!
They will base their diagnosis on your:
- history,
- symptom behaviour, and
- clinical tests.
In some cases, an MRI may be recommended by your health practitioner. Achilles tendons will often have a painful and prominent lump within the tendon.
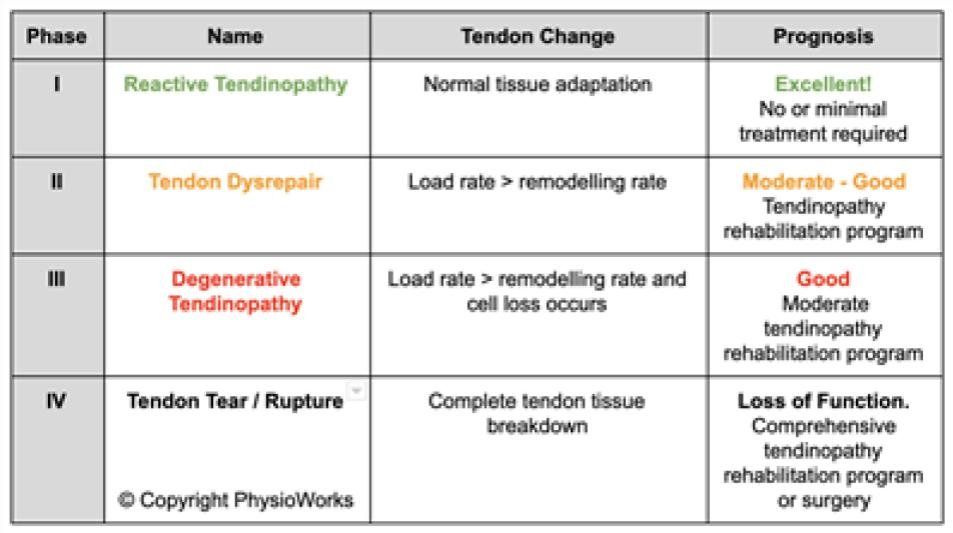
Tendinopathy Phases
How Is Achilles Tendinopathy Diagnosed?
Tendinopathy is a continuum of pathological processes and your treatment plan can be aided by correct identification of the current phase of injury and the application of appropriate exercise in the rehabilitation of your injury. Inappropriate loading may delay your recovery and your return to sport.
Identification of the phase helps to identify an entry point for your rehabilitation and how much you can perform in your recovery and balancing your activity levels in your rehabilitation plan.
It is very important to have your tendinopathy professionally assessed to identify your injury phase. Identifying your tendinopathy phase is also vital to direct your most effective treatment since certain modalities or exercises should only be applied or undertaken in specific tendon healing phases.
How Do You Treat Achilles Tendinopathy?
Achilles tendinopathy treatment varies significantly from how we treated the condition just a few years ago. Researchers are constantly updating their treatment recommendations. Based upon that our Achilles tendinopathy treatment protocols are regularly being updated to the latest research-supported versions.
Achilles tendinopathy treatment has progressed significantly in recent years. Based on this, it is now more important than ever to be assessed and treated by a physiotherapist who is up-to-date in the latest Achilles tendinopathy research findings and treatment strategies.
Achilles tendinopathy treatment is complex due to the high level of recurrence and patient variables. Achilles treatment also varies depending upon where you are within the tendon injury phase continuum as outlined above. The secret to a quick path to success is correctly assessing which phase you are currently and prescribe the appropriate exercises and advise suitable for that phase. That's exactly where the support of an up-to-date Achilles physiotherapist can fast-track your rehabilitation success.
How Is Your Rehabilitation Progress Monitored?
Your physiotherapist is highly skilled in the management of Achilles tendinopathy and your subsequent safe return to sport. Among other tests, your physiotherapist will use your pain provocation tests, strength measures, and functional activities as an effective tool to monitor your pain, function and when to progress exercises or return to sport.
They’ll also be happy to discuss your injury rehabilitation with your coach.
Exercise!
There is increasing importance in exercise in the management of tendinopathy. Isometric exercise, or exercise that the joint angle and muscle length do not change during exercise, have proven effects at pain relief for athletes suffering from tendinopathy.
How Will Your Physiotherapist Progress Your Treatment?
Tendinopathy treatment is progressed based on your tendon’s ability to withstand your exercises load. For most athletes, the traffic light system is utilised in order to clearly define how much training is too much.
Red will indicate that you need to reduce your exercise load. Amber indicates that you can exercise at current loads. Green indicates that you can safely increase your exercise loads.
Your physiotherapist will explain how to interpret your symptoms and plan your exercise loads based upon their assessment and your symptoms.
Managing Your Activity Load Is a Priority!
Exercise load management is vital to the successful treatment of an Achilles tendinopathy. Mild load increases will stimulate new tendon growth. Overload leads to tendinopathy deterioration.
Reduce the load to a level that allows the tendon to recover. In severe cases, this may mean total rest from your sport or modifying training depending on the severity of tendinopathy. Your activity load should be discussed with your physiotherapist, who will plan and modify your program accordingly, based upon your pain provocation tests, traffic light response to activity and other symptoms.
When managing load you should be guided by how the tendon responds not just immediately but also 24 hours later. Tendons are known to have a latent response to loading. This means they can take 24 hours or more to react. It is important to modify your activity to remain pain-free during and for following 24 to 48 hours.
How Long Does it Take for Achilles Tendinopathy to Heal?
If you identify your Achilles tendon injury in the early stages then load management and reduction will allow the tendon time to adapt and quickly recover. The reactive stage can be relatively short. Pain may settle in 5 to 10 days but the tendon will still be sensitive to high loads and training needs to be progressed gradually to prevent relapse. It is important that it does not progress into late stage 2 or stage 3 tendinopathy. These tendinopathies require additional time and rehabilitation.
A likely return to sport is in the order of 12 weeks. However, everyone is very different!
There is no specific time frame for when to progress from each stage to the next. Your Achilles tendonitis rehabilitation status will be determined by many factors during your physiotherapist’s clinical assessment and reviews. You’ll find that in most cases, your physiotherapist will seamlessly progress between the rehabilitation phases as your clinical assessment and function improves.
It is also important to note that each progression must be carefully monitored as attempting to progress too soon to the next level can lead to re-injury and frustration. The severity of your tendon injury, your compliance with treatment and the workload that you need to return to will ultimately determine how long your injury takes to successfully rehabilitate.
When Will Your Achilles Tendinopathy Heal?
Some practitioners suggest that the prognosis with guided treatment can be summed up by the tendinopathy phase:
- Phase I: days
- Phase II: weeks
- Phase III: months
- Phase IV: years
Exercises to Avoid with Achilles Tendinopathy
Avoid exercises that provoke your pain such as running up hills or stairs, sprinting, jumping, hopping and deep squats until advised otherwise by your physiotherapist.
Massage, Foam Rollers & Stretches
Massage or foam rolling of your calves, shins, quadriceps, ITB, and hamstrings, may assist in cases of Achilles tendinopathy. You can perform these in positions that do not hyper dorsiflex your ankle. Ask your physiotherapist for specific advice.
Eccentric Strengthening
Eccentric exercises were for many years the "go-to" exercises for tendinopathy rehabilitation. While definitely important, premature or overloaded eccentric exercises can delay your rehabilitation. Your physiotherapist will guide you when appropriate to commence strengthening that does not aggravate your Achilles tendinopathy. They may start you with isometrics that avoid tendon compression and progress from there towards a basic and then advance eccentric exercise program.
Adjacent Joints & Lower Limb Biomechanics
Researchers have identified several lower limb biomechanical issues may predispose you to Achilles tendinopathy. Your physiotherapist will assess things such as your ankle dorsiflexion, single-leg squat alignment and control, gluteal control, hip/knee bend ratio and running and landing technique. They’ll advise you if you require some treatment to address any deficiencies.
Other Treatments
Novel therapies such as the injection of sclerosing agents, platelet-derived growth factor (PDGF), and autologous blood into diseased tendons have shown potentially promising results, but more clinical trials are needed, so it is still considered experimental at this time. Your physiotherapist is happy to discuss these options with you when they consider them an appropriate treatment option.
Remember, all tendinopathies are different. Please seek the advice of your physiotherapist to determine the best rehabilitation appropriate to your tendinopathy.
Can Your Achilles Tendon Rupture?
The worst-case scenario is a total rupture of your Achilles tendon, which occurs when tendon cell death occurs and the tendon strength is insufficient. Treatment, in this case, may require surgery, plaster or a wedged walking boot for at least six weeks. Most of these injuries take six months or more to adequately rehabilitate, so avoiding Achilles tendon rupture remains the best option.
The best advice is to seek early advice from your physiotherapist to do all you can to avoid this nasty rupture happening in the first place.
Treatment Process
Preparation for Surgery
- Provide a complete list of your medications so you can be advises which to stopped prior to surgery,
- Treat any tooth, gum, bladder or bowel problems before surgery to reduce the risk of infection
- Stop anti-inflammatory medications (NSAIDs) at least seven days before the procedure.
- Stop or cut down smoking to reduce your surgery risks and improve your recovery
- Consider losing weight (if overweight) before surgery
Day of Surgery
- Report any infections to me prior to surgery as the procedure cannot be performed until all infections have cleared up.
- Do not consume alcohol - 24 hours prior to treatment,
- Do not eat or drink anything, including water, for 6 hours before surgery
- Avoid vigorous physical activity or exercise 24 hours prior to surgery,
During Surgery
- Administration of general anesthesia or sedation and local anesthesia
- The entire procedure can take 60 minutes to two hours.
- Procedure is performed and sent to recovery room, for observation
- Pain medications are prescribed to help with pain during the recovery phase.
After Surgery
- Do not consume large amounts of alcohol after surgery,
- Avoid vigorous physical activity or exercise until advised,
- Follow the Post Surgery Treatment Plan proscribed by the surgeon and post op care specialists.
- Any questions or complications should be communicated directly to the surgeon
Common Questions
If you have a specific question about your treatment, we recommend contacting the clinic