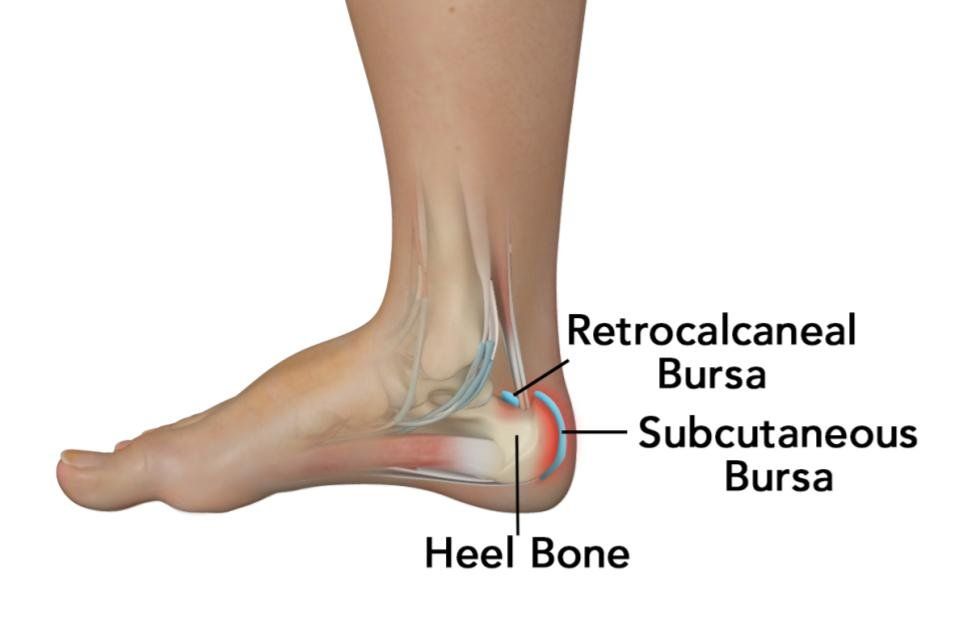
Retrocalcaneal Bursitis
What Is the Achilles Tendon?
The Achilles Tendon is the large tendon that connects the calf muscles to the heel bone (calcaneus) and is used when you walk, run, and jump.
What Is the Achilles Tendon Bursitis?
The retrocalcaneal bursa, a fluid-filled sac, which is located at the back of the heel under the Achilles tendon, contains a lubricating fluid that acts as a cushion to reduce friction between muscle and bones.
Achilles tendon bursitis or retrocalcaneal bursitis is a painful condition caused by swelling of the bursa.
Who Does Achilles Tendon Bursitis Affect?
Achilles tendon bursitis commonly occurs in athletes.
Also, children who suddenly increase their level of physical activity are at a higher risk of developing Achilles tendon bursitis.
Causes of Achilles Tendon Bursitis
Achilles tendon bursitis is caused by overuse of the ankle, which results in irritation and inflammation of the bursa. The common causes include:
- Too much of walking,
- Repeated jumping or
- Long-distance running.
Achilles tendon bursitis can also occur in conjunction with Achilles Tendinitis, the inflammation of the Achilles tendon.
Achilles Tendon Bursitis can be a secondary injury associated with chronic conditions such as:
- Plantar Fasciitis
- Heel Spurs
- Fibromyalgia
- Rheumatoid arthritis.
Symptoms of Achilles Tendon Bursitis
The most common symptom is pain and tenderness at the back of the heel, especially while walking or running.
Pain increases when standing on tiptoe. In some cases, the skin at the back of the heel may become warm and red.
Prevention of Achilles Tendon Bursitis
Achilles Tendon Bursitis may be prevented by maintaining proper form during exercises.
Ensure some warm-up exercises are performed before starting any sports activity, which may help prevent injury of the Achilles tendon.
Diagnosis of Achilles Tendon Bursitis
Your doctor may diagnose the condition based on:
- your symptoms
- a physical examination of the ankle.
Further examination of the foot can be very important, particularly for subtle injuries which require a high index of suspicion.
Diagnostic tests such as X-ray and MRI may be required later if the treatment does not improve the symptoms.
Treatment for Achilles Tendon Bursitis
Non-Surgical Treatment of Achilles Tendon Bursitis
The initial treatment for Achilles tendon bursitis includes:
- Restriction of activities that cause pain.
- Application of ice on the injured area, which will help to reduce the swelling. Ice should be wrapped in a cloth and applied rather than direct application.
- Non-steroidal anti-inflammatory medications may be given to reduce inflammation and pain.
- Custom heel wedges can be used to reduce the stress on the heel.
- Physical therapy may be recommended to help restore and improve the flexibility and strength of the muscles, tendons and joints around the ankle.
If retrocalcaneal bursitis is associated with Achilles Tendonitis, it may be necessary to immobilise the ankle for several weeks until healing takes place.
This can be done by applying a cast on the ankle, which limits ankle movement and allows the tendon to rest.
Surgical Treatment of Achilles Tendon Bursitis
Surgery is considered only when non-surgical treatments fail to resolve pain and inflammation.
Bursectomy
Bursectomy is a surgical procedure done to remove an inflamed or infected bursa.
Untreated Achilles Tendon Bursitis
Untreated Achilles Tendon Bursitis can lead to prolonged discomfort, tendon tears or rupture.
A rupture of the tendon will most likely require more serious treatment options, including casting or surgery.
Treatment Process
Preparation for Surgery
- Provide a complete list of your medications so you can be advises which to stopped prior to surgery,
- Treat any tooth, gum, bladder or bowel problems before surgery to reduce the risk of infection
- Stop anti-inflammatory medications (NSAIDs) at least seven days before the procedure.
- Stop or cut down smoking to reduce your surgery risks and improve your recovery
- Consider losing weight (if overweight) before surgery
Day of Surgery
- Report any infections to me prior to surgery as the procedure cannot be performed until all infections have cleared up.
- Do not consume alcohol - 24 hours prior to treatment,
- Do not eat or drink anything, including water, for 6 hours before surgery
- Avoid vigorous physical activity or exercise 24 hours prior to surgery,
During Surgery
- Administration of general anesthesia or sedation and local anesthesia
- The entire procedure can take 60 minutes to two hours.
- Procedure is performed and sent to recovery room, for observation
- Pain medications are prescribed to help with pain during the recovery phase.
After Surgery
- Do not consume large amounts of alcohol after surgery,
- Avoid vigorous physical activity or exercise until advised,
- Follow the Post Surgery Treatment Plan proscribed by the surgeon and post op care specialists.
- Any questions or complications should be communicated directly to the surgeon
Common Questions
If you have a specific question about your treatment, we recommend contacting the practice.